Health
Report on Chronic Pain Aims to Transform Understanding of Invisible Illnesses

A 2021 report supported by Health Canada has the potential to significantly reshape how the medical community addresses chronic pain, particularly among women suffering from invisible illnesses. Released during the peak of the COVID-19 pandemic, this report garnered little attention, but advocates and medical professionals are now urging for increased awareness and implementation of its findings.
Chronic pain conditions, including endometriosis, fibromyalgia, and other autoimmune diseases, often go unrecognized, leaving many patients without proper care. Women, in particular, face an uphill battle in being believed and diagnosed accurately. Conditions like endometriosis, where tissue similar to the uterine lining grows outside the uterus, can cause debilitating pain, yet often remain underdiagnosed.
For instance, Shae-Lynn Bakaluk from Moose Jaw endured over a decade of severe pain before receiving a diagnosis of endometriosis. Since her first menstrual period at age 10, she experienced pain so intense that she described it as “razors” or “barbed wire” wrapped around her organs. Bakaluk’s struggle highlights the tragic consequences of being dismissed by medical professionals, as she faced skepticism about the validity of her pain.
“I would try and run in gym class, and if I was on my period, I would fall over in pain,” Bakaluk recounted. “Teachers would say, ‘Oh, you’re just making things up.’” Over the years, she attended approximately 50 medical appointments, only to be told repeatedly that nothing was medically wrong. This lack of validation not only exacerbated her physical suffering but also led to feelings of isolation, anxiety, and depression.
The intersection of chronic pain and mental health issues is a recurring theme among those suffering from invisible illnesses. Bakaluk experienced suicidal thoughts, not as a desire to end her life, but as a response to overwhelming pain. “The more pain I was in, the more I needed pain medication,” she explained, only to be accused of seeking drugs rather than genuine relief.
Dr. Sony Singh, a representative from the Society of Obstetricians and Gynaecologists of Canada, acknowledged the systemic failure in addressing the needs of women with chronic pain. He emphasized that women experiencing such pain often feel dismissed and labeled as “crazy” by healthcare providers. This gender bias has deep roots in medical practice, leading to inequitable treatment for women, especially women of color, who face additional barriers in accessing care.
Bakaluk eventually received a correct diagnosis at age 21 when doctors discovered a benign ovarian tumor during surgery. It was during this procedure that endometriosis lesions were identified, offering her some much-needed validation. “After all these years, just to have a little bit of belief … I started bawling when he told me,” she said.
Another patient, Amanda Gibson, began experiencing alarming symptoms in 2020, including electric shocks, skin sensitivity, and persistent fatigue. Initially dismissed by doctors, she was advised to take antidepressants despite her insistence that her symptoms were physical. After multiple consultations, doctors suggested she might have fibromyalgia, a condition characterized by widespread pain and fatigue, often accompanied by cognitive difficulties.
Dr. Andrea Furlan, an associate professor at the University of Toronto, commented on the stigma surrounding women’s health issues. She noted that many with fibromyalgia appear outwardly “normal,” which can lead to disbelief about their pain. “We carry so much guilt and burden,” Gibson remarked, underscoring the need for better understanding and support for women in the healthcare system.
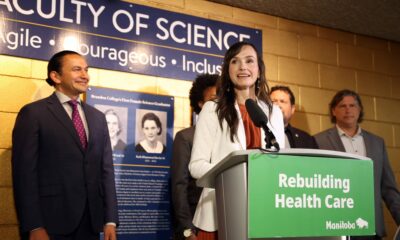
The Canadian Pain Task Force was established in 2019 to address these issues, leading to a national consultation aimed at improving the recognition and treatment of chronic pain. The task force released its recommendations in March 2021, but the report’s visibility was overshadowed by the ongoing pandemic and political upheaval in Canada.
Maria Hudspith, co-chair of the Canadian Pain Task Force, expressed frustration over the report’s lack of attention. “It’s having a huge impact on people’s lives, but it’s still not seen,” she stated. The healthcare system often seeks to identify an underlying cause for pain rather than addressing pain itself, leaving many patients without adequate support.
The need for education in recognizing and treating chronic pain has never been more critical. According to statistics from the task force, individuals living with chronic pain are four times more likely to experience depression and anxiety and are twice as likely to contemplate suicide compared to the general population.
Dr. Singh pointed out that the healthcare system has largely failed to acknowledge the catastrophic impact of chronic pain conditions, particularly in relation to the menstrual cycle. Recent updates to medical curricula in Canadian medical schools aim to improve understanding of pain management and diagnosis, but much work remains to be done.
As awareness grows around these issues, the hope is that the insights from the Canadian Pain Task Force will lead to better support systems for individuals suffering from chronic pain, particularly women. Hudspith, alongside other advocates, continues to push for recognition and action to ensure that the pain experienced by many is validated and treated with the seriousness it deserves.
-
 Education3 months ago
Education3 months agoBrandon University’s Failed $5 Million Project Sparks Oversight Review
-

 Science4 months ago
Science4 months agoMicrosoft Confirms U.S. Law Overrules Canadian Data Sovereignty
-

 Lifestyle3 months ago
Lifestyle3 months agoWinnipeg Celebrates Culinary Creativity During Le Burger Week 2025
-

 Health4 months ago
Health4 months agoMontreal’s Groupe Marcelle Leads Canadian Cosmetic Industry Growth
-

 Technology4 months ago
Technology4 months agoDragon Ball: Sparking! Zero Launching on Switch and Switch 2 This November
-

 Science4 months ago
Science4 months agoTech Innovator Amandipp Singh Transforms Hiring for Disabled
-

 Education3 months ago
Education3 months agoRed River College Launches New Programs to Address Industry Needs
-

 Technology4 months ago
Technology4 months agoGoogle Pixel 10 Pro Fold Specs Unveiled Ahead of Launch
-

 Business3 months ago
Business3 months agoRocket Lab Reports Strong Q2 2025 Revenue Growth and Future Plans
-

 Technology2 months ago
Technology2 months agoDiscord Faces Serious Security Breach Affecting Millions
-

 Education3 months ago
Education3 months agoAlberta Teachers’ Strike: Potential Impacts on Students and Families
-
 Science4 months ago
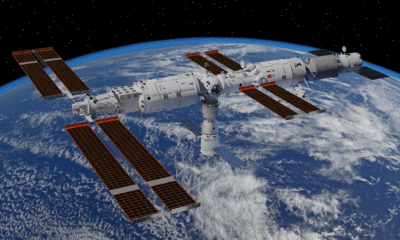
Science4 months agoChina’s Wukong Spacesuit Sets New Standard for AI in Space
-

 Education3 months ago
Education3 months agoNew SĆIȺNEW̱ SṮEȽIṮḴEȽ Elementary Opens in Langford for 2025/2026 Year
-

 Technology4 months ago
Technology4 months agoWorld of Warcraft Players Buzz Over 19-Quest Bee Challenge
-

 Business4 months ago
Business4 months agoNew Estimates Reveal ChatGPT-5 Energy Use Could Soar
-

 Business3 months ago
Business3 months agoDawson City Residents Rally Around Buy Canadian Movement
-

 Technology2 months ago
Technology2 months agoHuawei MatePad 12X Redefines Tablet Experience for Professionals
-

 Business3 months ago
Business3 months agoBNA Brewing to Open New Bowling Alley in Downtown Penticton
-

 Technology4 months ago
Technology4 months agoFuture Entertainment Launches DDoD with Gameplay Trailer Showcase
-

 Technology4 months ago
Technology4 months agoGlobal Launch of Ragnarok M: Classic Set for September 3, 2025
-

 Technology4 months ago
Technology4 months agoInnovative 140W GaN Travel Adapter Combines Power and Convenience
-

 Science4 months ago
Science4 months agoXi Labs Innovates with New AI Operating System Set for 2025 Launch
-

 Top Stories2 months ago
Top Stories2 months agoBlue Jays Shift José Berríos to Bullpen Ahead of Playoffs
-

 Technology4 months ago
Technology4 months agoNew IDR01 Smart Ring Offers Advanced Sports Tracking for $169










