Top Stories
Ontario Doctors Urge Overhaul of In-Home Nursing for Palliative Care

Concerns about the quality of in-home nursing care for dying patients in Ontario have prompted two local doctors to advocate for significant changes. After seven years of providing palliative care in the Grey-Bruce region, Dr. Alexandra Hodgson decided to shift her focus away from in-home care due to persistent issues with the Victorian Order of Nurses (VON). “I couldn’t leave a patient’s home anymore with the stress and anxiety of not knowing what was going to happen to that person until I came back in a week,” she explained.
Dr. Hodgson’s decision comes amidst growing frustrations from healthcare professionals regarding the nursing services provided by VON, which they claim often puts vulnerable patients at risk. She now primarily works in hospice and hospital settings in Owen Sound, Ontario, where she believes she can offer safer care.
In a similar vein, Dr. Susan Batten, another palliative care specialist in the region, has voiced her concerns about VON’s ability to adequately support complex palliative patients. In a letter to Ontario Health AtHome, which manages home care services, she stated, “I will no longer be able to support palliative patients in their home if they are supported with VON nursing care.” Both doctors are calling for changes to ensure safe and effective nursing support for patients in their final days.
The challenges faced by Hodgson and Batten are reflective of broader issues within Ontario’s home care system. Many patients prefer to die at home, but inadequate nursing support has made this increasingly difficult. According to reports, VON is not the only provider in the region, yet both doctors assert that VON has consistently failed to meet acceptable standards of care.
In their experience, effective in-home care relies on strong communication between nurses and doctors. However, both Hodgson and Batten have noted persistent communication failures in homes served by VON. Batten highlighted that when the system functions well, nurses visit frequently and have 24-hour access to medical professionals. This vital exchange of information is often lacking when VON nurses are involved.
The disparity in care quality between VON and another service provider, CarePartners, is striking. Batten remarked, “What I know is that CarePartners does this well and VON does not.” She pointed out that VON has not met the standards of palliative care since she began working in the field in 2013.
Both doctors outlined several persistent problems with VON’s nursing services. These include incomplete patient assessments, inadequate symptom tracking, and improper medication management. In one instance, Batten described how a patient suffered from pain for days due to a disconnected medication pump, an issue that could have been avoided with better oversight.
Furthermore, the lack of accessible and comprehensive patient charting has exacerbated these challenges. Basic information like blood pressure readings often goes unrecorded, leading to inefficiencies that hinder effective patient care. The absence of quality control measures similar to those found in hospitals and hospice settings has left both doctors concerned about the level of care provided by VON.
In response to these allegations, VON released a statement asserting that they take concerns seriously and are committed to improving communication and coordination with healthcare providers. The organization emphasized its dedication to delivering integrated care for all clients.
Both Hodgson and Batten acknowledge that VON nurses often work under challenging conditions, facing lower pay compared to hospital staff and long travel distances in rural areas. Despite these challenges, they argue that better transparency and accountability in the oversight of home care contracts are essential for improving care quality.
Hodgson expressed frustration at the disparity between the two organizations operating in the same geographical area, questioning why one performs significantly better than the other.
The Ontario New Democratic Party (NDP) has also weighed in on the situation, with health critic France Gélinas asserting that the competitive bidding process for nursing contracts contributes to declining care quality. “The companies try to out-bid each other on price and that’s not how quality health care is provided,” she stated. Gélinas’s office reportedly receives continual complaints regarding the home care system, which she described as “broken.”
As Ontario grapples with these issues, the future of in-home palliative care remains uncertain. Both Hodgson and Batten’s experiences highlight an urgent need for reform in the province’s approach to home nursing services, particularly for the most vulnerable patients at the end of their lives.
-
 Education5 months ago
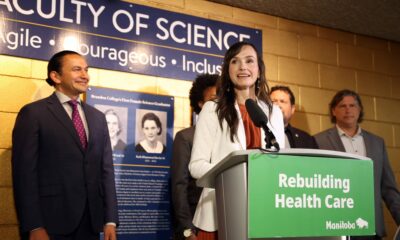
Education5 months agoBrandon University’s Failed $5 Million Project Sparks Oversight Review
-

 Science6 months ago
Science6 months agoMicrosoft Confirms U.S. Law Overrules Canadian Data Sovereignty
-

 Lifestyle5 months ago
Lifestyle5 months agoWinnipeg Celebrates Culinary Creativity During Le Burger Week 2025
-

 Health6 months ago
Health6 months agoMontreal’s Groupe Marcelle Leads Canadian Cosmetic Industry Growth
-

 Education5 months ago
Education5 months agoNew SĆIȺNEW̱ SṮEȽIṮḴEȽ Elementary Opens in Langford for 2025/2026 Year
-

 Science6 months ago
Science6 months agoTech Innovator Amandipp Singh Transforms Hiring for Disabled
-

 Technology6 months ago
Technology6 months agoDragon Ball: Sparking! Zero Launching on Switch and Switch 2 This November
-

 Business2 months ago
Business2 months agoEngineAI Unveils T800 Humanoid Robot, Setting New Industry Standards
-
 Technology3 weeks ago
Technology3 weeks agoDigg Relaunches as Founders Kevin Rose and Alexis Ohanian Join Forces
-

 Top Stories2 months ago
Top Stories2 months agoCanadiens Eye Elias Pettersson: What It Would Cost to Acquire Him
-

 Education6 months ago
Education6 months agoRed River College Launches New Programs to Address Industry Needs
-

 Business5 months ago
Business5 months agoRocket Lab Reports Strong Q2 2025 Revenue Growth and Future Plans
-

 Technology6 months ago
Technology6 months agoGoogle Pixel 10 Pro Fold Specs Unveiled Ahead of Launch
-

 Education6 months ago
Education6 months agoAlberta Teachers’ Strike: Potential Impacts on Students and Families
-

 Technology4 months ago
Technology4 months agoDiscord Faces Serious Security Breach Affecting Millions
-

 Business6 months ago
Business6 months agoBNA Brewing to Open New Bowling Alley in Downtown Penticton
-
 Science6 months ago
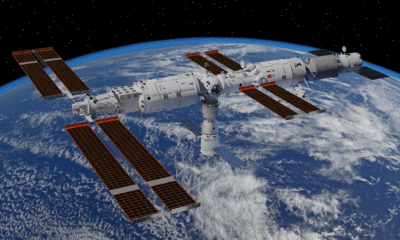
Science6 months agoChina’s Wukong Spacesuit Sets New Standard for AI in Space
-

 Lifestyle4 months ago
Lifestyle4 months agoCanadian Author Secures Funding to Write Book Without Financial Strain
-

 Business6 months ago
Business6 months agoNew Estimates Reveal ChatGPT-5 Energy Use Could Soar
-

 Business1 month ago
Business1 month agoNvidia and AMD CEOs Unveil AI Innovations at CES 2026
-

 Business4 months ago
Business4 months agoHydro-Québec Espionage Trial Exposes Internal Oversight Failures
-

 Top Stories4 months ago
Top Stories4 months agoPatrik Laine Struggles to Make Impact for Canadiens Early Season
-

 Business6 months ago
Business6 months agoDawson City Residents Rally Around Buy Canadian Movement
-

 Technology6 months ago
Technology6 months agoFuture Entertainment Launches DDoD with Gameplay Trailer Showcase










