Health
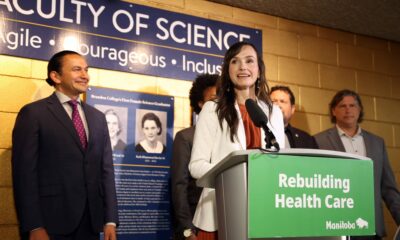
Brandon’s Mental Health Services Face Scrutiny After Decades

Concerns over mental health services in Brandon, Manitoba, have resurfaced as stakeholders evaluate the community’s evolving needs. The closure of the Brandon Mental Health Centre (BMHC) in the late 1990s aimed to reduce stigma and integrate care into the community. However, many residents now question whether this approach has effectively met the escalating demand for mental health support.
When the BMHC was closed, the intention was to shift care from institutional settings to community-based services. Former health minister Jim McCrae emphasized this shift in a 2005 op-ed, stating that it offered a better chance for successful outcomes. “Before the reforms, people had to go to BMHC to get help. The stigma was too overwhelming and intimidating,” he wrote. The closure was accompanied by promises of increased funding and support networks, but the reality has diverged sharply from these goals.
Since the BMHC’s closure, several organizations have taken on the responsibility of mental health care in Brandon and western Manitoba. This includes the establishment of the Centre for Adult Psychiatry at the Brandon Regional Health Centre and the Children and Adolescent Treatment Centre. Despite these initiatives, many healthcare professionals argue that the system is struggling to keep pace with the rising demand for services.
The downtown area, where many social services are concentrated, has faced deterioration. Local residents and business owners have voiced concerns that this concentration contributes to public safety issues and a perception of disorder. A report released by the Brandon Police Service in September 2023 highlighted the need for a crisis response unit that pairs police officers with mental health professionals, a move intended to improve the safety and efficacy of responses to mental health crises.
Insp. Dana McCallum of the Brandon Police Service remarked, “I think it’ll be very beneficial to actually have trained professionals dealing with those mental health calls.” The report also identified significant gaps in available mental health resources, including a lack of detox beds and long-term stabilization options. Officers have noted that they often discharge individuals into the community without adequate follow-up or housing, exacerbating existing challenges.
One of the report’s key recommendations is to decentralize social services to alleviate the burden on the downtown area. In addition, the police suggested the creation of a dedicated mental health hospital or recovery centre, similar to the one that was closed nearly three decades ago. This proposal underscores growing concerns that the community-based approach has not sufficiently addressed the needs of those seeking help.
Concerns regarding the effectiveness of the current mental health system have been echoed by local health professionals. Dr. Derry Decter criticized the lack of funding for necessary supports following the BMHC’s closure, stating, “People once cared for were abandoned, left to their own devices in a violent world of uncontrolled access to alcohol and drugs.” His comments reflect a broader sentiment that the transition from institutional care has not occurred as intended.
The Westwind Counselling and Eating Disorder Recovery Centre, established by former BMHC staff, recently closed its local operations, further illustrating the challenges facing mental health services in the region. At its peak, the centre charged clients upwards of $20,000 for a three-month stay, raising questions about accessibility and affordability in mental health care.
With ongoing recruitment efforts for at least four family physicians to support psychiatric services, the community is urged to reconsider how mental health services are delivered. Many believe that a serious examination of current practices is overdue.
As Brandon navigates these complex challenges, it is evident that a collaborative approach involving healthcare professionals, law enforcement, and community stakeholders is essential to reshape the future of mental health services. The time has come for meaningful dialogue and action to ensure that all residents receive the care they need and deserve.
-
 Education2 months ago
Education2 months agoBrandon University’s Failed $5 Million Project Sparks Oversight Review
-

 Lifestyle3 months ago
Lifestyle3 months agoWinnipeg Celebrates Culinary Creativity During Le Burger Week 2025
-

 Science3 months ago
Science3 months agoMicrosoft Confirms U.S. Law Overrules Canadian Data Sovereignty
-

 Health3 months ago
Health3 months agoMontreal’s Groupe Marcelle Leads Canadian Cosmetic Industry Growth
-

 Science3 months ago
Science3 months agoTech Innovator Amandipp Singh Transforms Hiring for Disabled
-

 Technology3 months ago
Technology3 months agoDragon Ball: Sparking! Zero Launching on Switch and Switch 2 This November
-

 Education3 months ago
Education3 months agoRed River College Launches New Programs to Address Industry Needs
-

 Technology3 months ago
Technology3 months agoGoogle Pixel 10 Pro Fold Specs Unveiled Ahead of Launch
-

 Technology1 month ago
Technology1 month agoDiscord Faces Serious Security Breach Affecting Millions
-

 Business2 months ago
Business2 months agoRocket Lab Reports Strong Q2 2025 Revenue Growth and Future Plans
-
 Science3 months ago
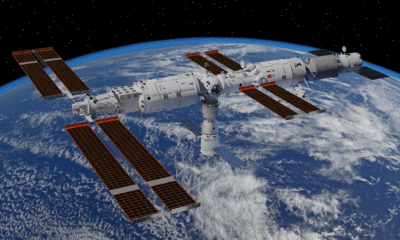
Science3 months agoChina’s Wukong Spacesuit Sets New Standard for AI in Space
-

 Education3 months ago
Education3 months agoAlberta Teachers’ Strike: Potential Impacts on Students and Families
-

 Technology3 months ago
Technology3 months agoWorld of Warcraft Players Buzz Over 19-Quest Bee Challenge
-

 Business3 months ago
Business3 months agoNew Estimates Reveal ChatGPT-5 Energy Use Could Soar
-

 Business3 months ago
Business3 months agoDawson City Residents Rally Around Buy Canadian Movement
-

 Education3 months ago
Education3 months agoNew SĆIȺNEW̱ SṮEȽIṮḴEȽ Elementary Opens in Langford for 2025/2026 Year
-

 Technology1 month ago
Technology1 month agoHuawei MatePad 12X Redefines Tablet Experience for Professionals
-

 Technology3 months ago
Technology3 months agoFuture Entertainment Launches DDoD with Gameplay Trailer Showcase
-

 Business3 months ago
Business3 months agoBNA Brewing to Open New Bowling Alley in Downtown Penticton
-

 Technology3 months ago
Technology3 months agoGlobal Launch of Ragnarok M: Classic Set for September 3, 2025
-

 Technology3 months ago
Technology3 months agoInnovative 140W GaN Travel Adapter Combines Power and Convenience
-

 Science3 months ago
Science3 months agoXi Labs Innovates with New AI Operating System Set for 2025 Launch
-

 Technology3 months ago
Technology3 months agoNew IDR01 Smart Ring Offers Advanced Sports Tracking for $169
-

 Technology3 months ago
Technology3 months agoDiscover the Relaxing Charm of Tiny Bookshop: A Cozy Gaming Escape










