Health
Brandon’s Mental Health Care Faces New Challenges After 30 Years

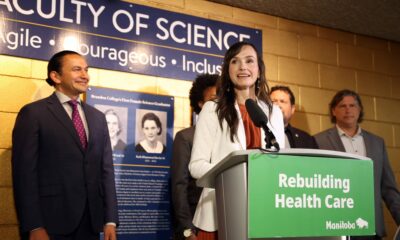
In a significant development for mental health care in Brandon, Manitoba, recent reports highlight ongoing challenges that have resurfaced nearly three decades after the closure of the Brandon Mental Health Centre. The shift from institutional care to community-based support, initially aimed at reducing stigma and improving access, has faced scrutiny as gaps in the system become increasingly evident.
The closure of the Brandon Mental Health Centre in the late 1990s was part of a broader reform strategy to move mental health services into the community. Officials, including former Progressive Conservative health minister Jim McCrae, championed this move as essential for modernizing care. In a 2005 op-ed, McCrae emphasized that the stigma associated with institutional care had prevented many individuals from seeking help, leading to significant suffering among those in need.
Despite these ambitious goals, the consolidation of mental health services has not produced the desired outcomes. While the transition included the establishment of several facilities, such as the Centre for Adult Psychiatry and the Children and Adolescent Treatment Centre, concerns have emerged regarding the adequacy of these services. Residents and service providers have noted a deterioration in the downtown area, where many mental health services are concentrated. This concentration has led to perceptions of disorder, prompting a call for more decentralized service delivery.
A recent report from the Brandon Police Service, released in September 2023, underscores these issues. Following consultations with community stakeholders, the report called for the creation of a crisis response unit that would pair police officers with mental health professionals. Insp. Dana McCallum stated, “It’ll be very beneficial to actually have trained professionals dealing with those mental health calls,” highlighting the need for expert intervention in crisis situations.
The report also pointed out systemic pressures that contribute to a perception of disorder in the downtown area. Officers reported facing significant challenges, including a lack of access to detox beds and mental health assessment facilities. The police found themselves discharging individuals without adequate follow-up or housing, exacerbating the situation. “The entire region funnels into Brandon and then stops downtown,” the report noted, emphasizing the need for a comprehensive approach to mental health care.
Among the recommendations proposed by the police was the establishment of a dedicated mental health hospital or recovery centre, reminiscent of the services that existed prior to the closure of the Brandon Mental Health Centre. This suggestion raises critical questions about the effectiveness of the current community-based model and whether it adequately meets the needs of individuals seeking mental health support.
Local health professionals have long expressed concerns about the state of mental health services in the region. Dr. Derry Decter has been vocal about the inadequacies of funding and support following the closure of the BMHC. In a letter to the editor in 2006, he stated, “People once cared for were abandoned, left to their own devices in a violent world of uncontrolled access to alcohol and drugs.” His words resonate with the ongoing struggles faced by many individuals in the community.
The closure of the Westwind Counselling and Eating Disorder Recovery Centre, which relocated to Kelowna, B.C., further illustrates the challenges within the system. In 2020, the counselling service charged clients upwards of $20,000 for a three-month stay, highlighting the financial barriers many face in accessing necessary care.
As the community grapples with these complex issues, it is evident that serious questions need to be addressed regarding the delivery of mental health services in Brandon. The time has come for stakeholders to collaborate and develop a more effective and inclusive system that can adequately support those in need. The situation calls for immediate attention to ensure that the mental health care landscape evolves to meet the demands of a growing and diverse population.
-
 Education3 months ago
Education3 months agoBrandon University’s Failed $5 Million Project Sparks Oversight Review
-

 Science4 months ago
Science4 months agoMicrosoft Confirms U.S. Law Overrules Canadian Data Sovereignty
-

 Lifestyle3 months ago
Lifestyle3 months agoWinnipeg Celebrates Culinary Creativity During Le Burger Week 2025
-

 Health4 months ago
Health4 months agoMontreal’s Groupe Marcelle Leads Canadian Cosmetic Industry Growth
-

 Science4 months ago
Science4 months agoTech Innovator Amandipp Singh Transforms Hiring for Disabled
-

 Technology4 months ago
Technology4 months agoDragon Ball: Sparking! Zero Launching on Switch and Switch 2 This November
-

 Education4 months ago
Education4 months agoRed River College Launches New Programs to Address Industry Needs
-

 Business3 months ago
Business3 months agoRocket Lab Reports Strong Q2 2025 Revenue Growth and Future Plans
-

 Technology4 months ago
Technology4 months agoGoogle Pixel 10 Pro Fold Specs Unveiled Ahead of Launch
-

 Technology2 months ago
Technology2 months agoDiscord Faces Serious Security Breach Affecting Millions
-

 Education4 months ago
Education4 months agoAlberta Teachers’ Strike: Potential Impacts on Students and Families
-

 Education4 months ago
Education4 months agoNew SĆIȺNEW̱ SṮEȽIṮḴEȽ Elementary Opens in Langford for 2025/2026 Year
-
 Science4 months ago
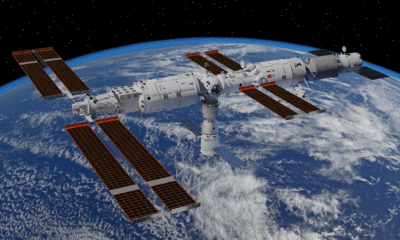
Science4 months agoChina’s Wukong Spacesuit Sets New Standard for AI in Space
-

 Business4 months ago
Business4 months agoBNA Brewing to Open New Bowling Alley in Downtown Penticton
-

 Business4 months ago
Business4 months agoNew Estimates Reveal ChatGPT-5 Energy Use Could Soar
-

 Technology4 months ago
Technology4 months agoWorld of Warcraft Players Buzz Over 19-Quest Bee Challenge
-

 Business4 months ago
Business4 months agoDawson City Residents Rally Around Buy Canadian Movement
-

 Technology2 months ago
Technology2 months agoHuawei MatePad 12X Redefines Tablet Experience for Professionals
-

 Top Stories3 months ago
Top Stories3 months agoBlue Jays Shift José Berríos to Bullpen Ahead of Playoffs
-

 Technology4 months ago
Technology4 months agoFuture Entertainment Launches DDoD with Gameplay Trailer Showcase
-

 Technology4 months ago
Technology4 months agoGlobal Launch of Ragnarok M: Classic Set for September 3, 2025
-

 Technology4 months ago
Technology4 months agoInnovative 140W GaN Travel Adapter Combines Power and Convenience
-

 Science4 months ago
Science4 months agoXi Labs Innovates with New AI Operating System Set for 2025 Launch
-

 Technology4 months ago
Technology4 months agoNew IDR01 Smart Ring Offers Advanced Sports Tracking for $169










