Health
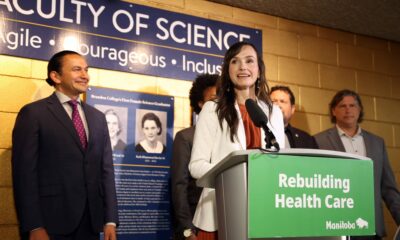
B.C. Health Care Needs Comprehensive Reform, Not Minor Adjustments

The government of British Columbia has announced preliminary findings from an administrative review of its health-care system, but many patients are left wondering if significant changes are on the horizon. The review, presented by the Eby government, highlighted some cost savings amounting to $60 million, which the government claims could be reinvested into frontline care. However, the chronic access issues affecting patients remain largely unaddressed.
Patients in British Columbia experienced a median wait time of 32.2 weeks for care last year, marking the longest wait on record. Additionally, those requiring diagnostic imaging faced median waits of over three months for a CT scan and nearly six months for an MRI. These staggering delays have prompted many B.C. residents to seek medical treatment outside Canada, underscoring the urgency of the situation.
Despite acknowledging these pressing issues, the Eby government has yet to propose any substantial reforms to the health-care system. The administrative review primarily focused on eliminating bureaucratic inefficiencies and creating a new shared service model to reduce administrative overlap among health regions. While these measures may streamline operations, they are unlikely to enhance patient care or access.
Rethinking Health Care Funding
To truly address the challenges facing its health-care system, British Columbia could look to successful models in countries such as Australia, Germany, the Netherlands, and Switzerland. These nations provide timely medical care and have more resources available, often while spending comparably or less than Canada on health care.
One key difference lies in the funding structure for hospitals. Currently, B.C. allocates a lump-sum budget to hospitals at the beginning of each fiscal year. This model creates disincentives for hospitals to treat more patients, as each new patient is perceived as a financial burden on the budget. By contrast, countries with more effective health-care systems typically reimburse hospitals based on the number of patients treated and the complexity of their conditions. This approach transforms each patient into a potential revenue source, encouraging hospitals to increase patient volume and improve care.
Research indicates that reforming hospital payment structures can lead to increased care volume, reduced costs per admission, and, crucially for British Columbians, shorter wait times. Lessons can be drawn not only from international examples but also from British Columbia’s own pilot project that tested this payment model from 2010 to 2013.
The lack of groundbreaking changes in the wake of the Eby government’s administrative review suggests that patients should not anticipate immediate improvements in their access to health care. Without a shift from administrative adjustments to comprehensive reforms, residents may continue to endure lengthy waits and seek alternatives outside the province.
Mackenzie Moir, a Senior Policy Analyst with the Fraser Institute, emphasizes the need for the B.C. government to prioritize meaningful reform. Until then, patients in British Columbia will likely remain at the mercy of a health-care system that has yet to fully embrace effective change.
-
 Education5 months ago
Education5 months agoBrandon University’s Failed $5 Million Project Sparks Oversight Review
-

 Science6 months ago
Science6 months agoMicrosoft Confirms U.S. Law Overrules Canadian Data Sovereignty
-

 Lifestyle5 months ago
Lifestyle5 months agoWinnipeg Celebrates Culinary Creativity During Le Burger Week 2025
-

 Health6 months ago
Health6 months agoMontreal’s Groupe Marcelle Leads Canadian Cosmetic Industry Growth
-

 Education5 months ago
Education5 months agoNew SĆIȺNEW̱ SṮEȽIṮḴEȽ Elementary Opens in Langford for 2025/2026 Year
-

 Science6 months ago
Science6 months agoTech Innovator Amandipp Singh Transforms Hiring for Disabled
-

 Technology6 months ago
Technology6 months agoDragon Ball: Sparking! Zero Launching on Switch and Switch 2 This November
-

 Business2 months ago
Business2 months agoEngineAI Unveils T800 Humanoid Robot, Setting New Industry Standards
-
 Technology3 weeks ago
Technology3 weeks agoDigg Relaunches as Founders Kevin Rose and Alexis Ohanian Join Forces
-

 Top Stories2 months ago
Top Stories2 months agoCanadiens Eye Elias Pettersson: What It Would Cost to Acquire Him
-

 Education6 months ago
Education6 months agoRed River College Launches New Programs to Address Industry Needs
-

 Business5 months ago
Business5 months agoRocket Lab Reports Strong Q2 2025 Revenue Growth and Future Plans
-

 Technology6 months ago
Technology6 months agoGoogle Pixel 10 Pro Fold Specs Unveiled Ahead of Launch
-

 Education6 months ago
Education6 months agoAlberta Teachers’ Strike: Potential Impacts on Students and Families
-

 Technology4 months ago
Technology4 months agoDiscord Faces Serious Security Breach Affecting Millions
-

 Business6 months ago
Business6 months agoBNA Brewing to Open New Bowling Alley in Downtown Penticton
-
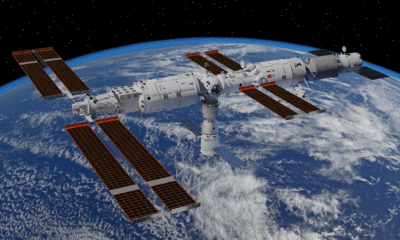
 Science6 months ago
Science6 months agoChina’s Wukong Spacesuit Sets New Standard for AI in Space
-

 Lifestyle4 months ago
Lifestyle4 months agoCanadian Author Secures Funding to Write Book Without Financial Strain
-

 Business6 months ago
Business6 months agoNew Estimates Reveal ChatGPT-5 Energy Use Could Soar
-

 Business1 month ago
Business1 month agoNvidia and AMD CEOs Unveil AI Innovations at CES 2026
-

 Business4 months ago
Business4 months agoHydro-Québec Espionage Trial Exposes Internal Oversight Failures
-

 Top Stories4 months ago
Top Stories4 months agoPatrik Laine Struggles to Make Impact for Canadiens Early Season
-

 Business6 months ago
Business6 months agoDawson City Residents Rally Around Buy Canadian Movement
-

 Technology6 months ago
Technology6 months agoFuture Entertainment Launches DDoD with Gameplay Trailer Showcase










